Measles Outbreak Inspires New Conversations About Vaccination With Families
Editor’s note: In the midst of several measles outbreaks in the U.S., AAP News reporters spoke with pediatricians about their experience with the disease and how they are talking to families about immunizations. These are some of their stories. The full article appeared in April 2025 AAP News and can be found online at aapnews.org.
Pediatricians across the country say the recent measles outbreak that led to the death of two children in Texas is changing the way families talk about vaccines.
Some families have asked to receive measles-mumps-rubella (MMR) vaccines early for their children, while others have canceled appointments out of fear of exposing their children to measles in a clinical setting, she said. Still other parents have refused vaccination, including families who previously vaccinated their children.
Alexandra J. Cvijanovich, M.D., M.Ed., FAAP, a general pediatrician in Albuquerque, N.M., said the outbreak has changed the way many families view vaccination. “I think for my fellow pediatricians, remember that every time you see a child is an opportunity to vaccinate,” Dr. Cvijanovich said. She also emphasizes that community immunity is going away as vaccination rates drop, so she emphasizes that immunization is the only way for parents to protect their children.
“The death of a child is always tragic, but it is particularly devastating when a child dies from a preventable injury and illness,” said Valerie B. Smith, M.D., M.P.H., FAAP, president of the Texas Pediatric Society (AAP Texas Chapter). “We know that MMR vaccination is safe, effective and can help stop the spread of measles and save lives. Pediatricians in Texas will continue to advocate for vaccination and provide access to the MMR vaccine as the most important way to keep children healthy and safe from measles.”
“I think for my fellow pediatricians, remember that every time you see a child is an opportunity to vaccinate.”
Alexandra J. Cvijanovich, M.D., M.Ed., FAAP
General Pediatrician


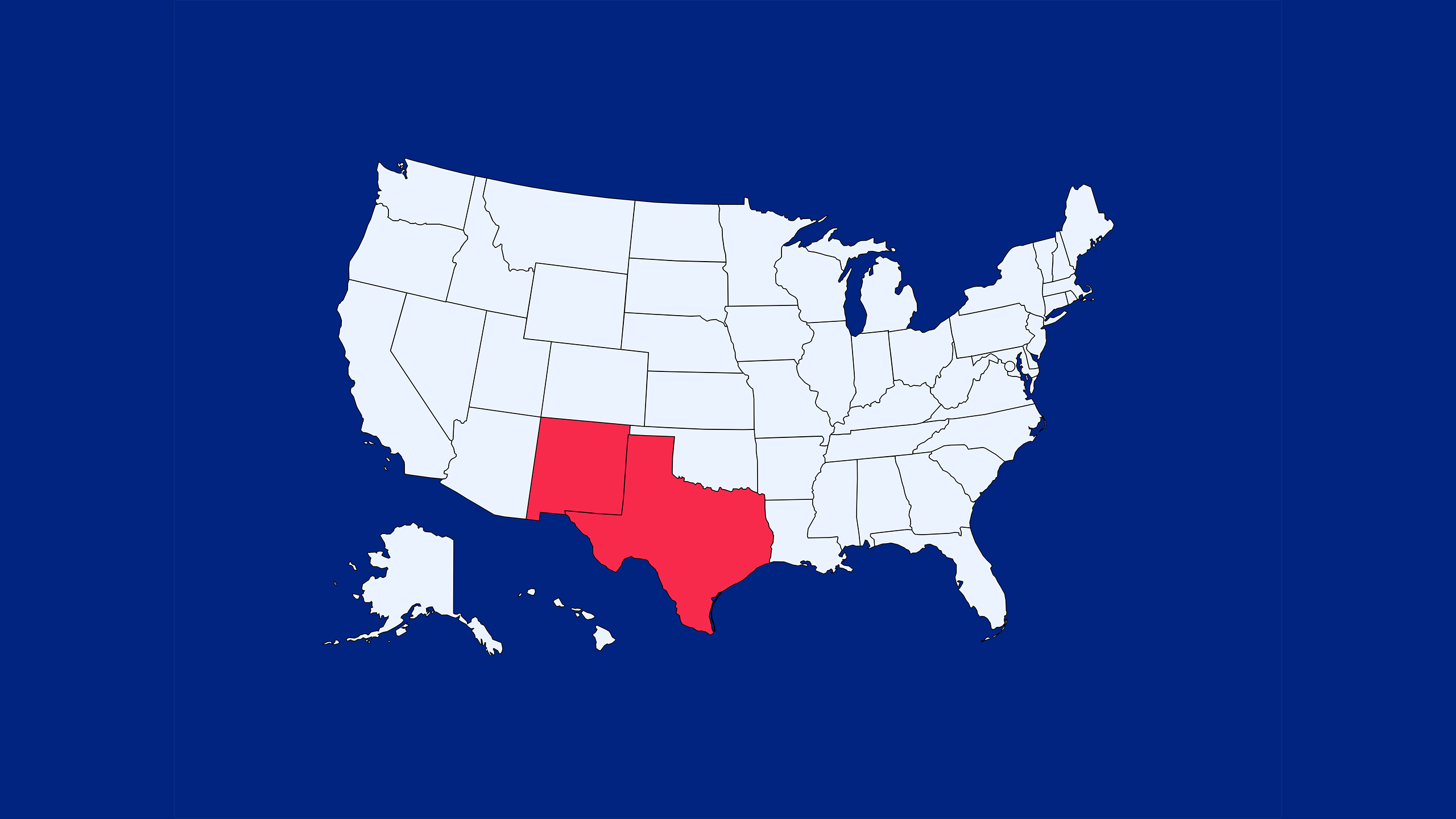
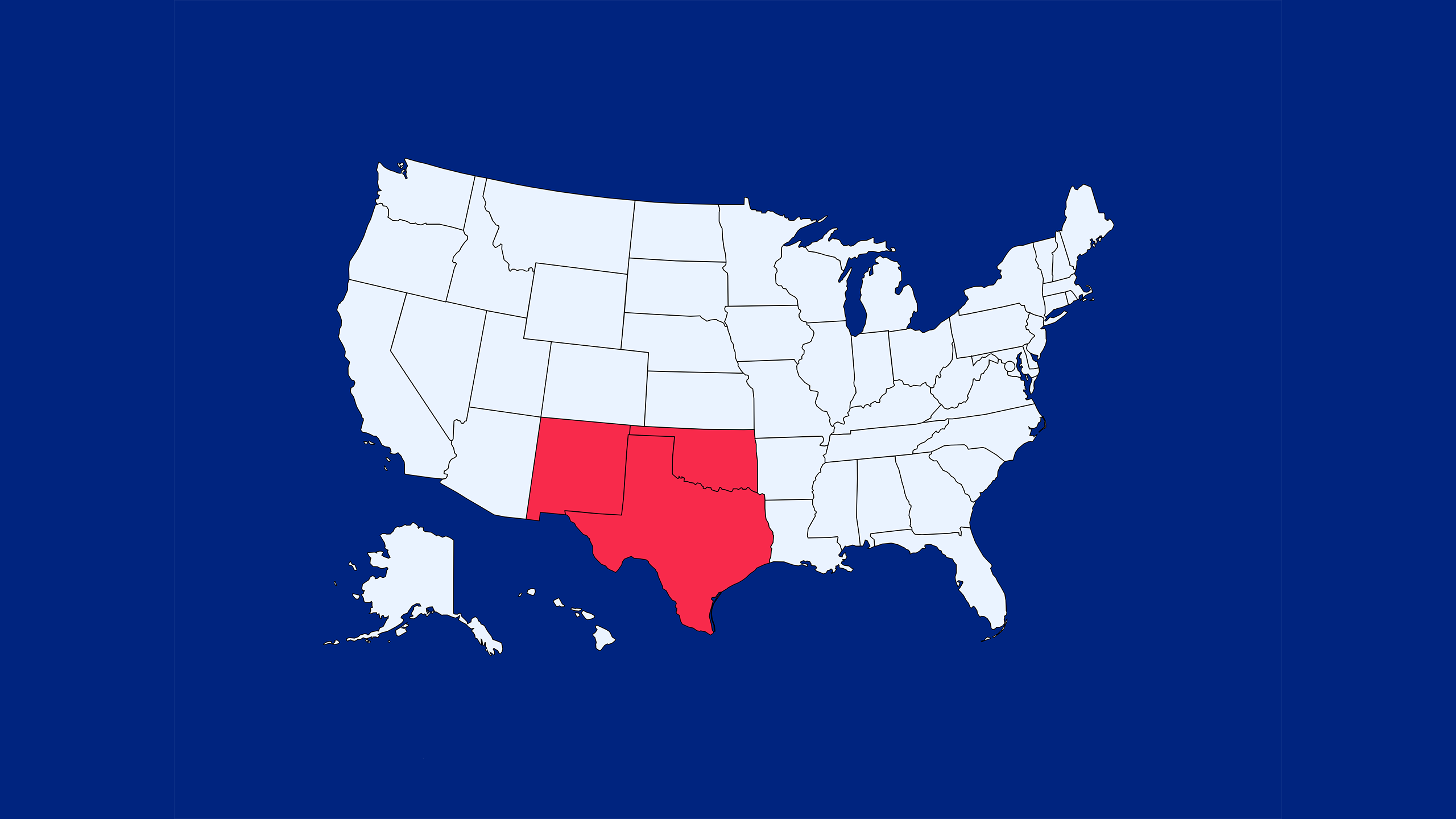
The CDC considers 95% vaccination rate as community immunity against measles. All cases in the affected states, shown in the map below, are since January 1, 2025. The CDC considers an outbreak to be three related cases.
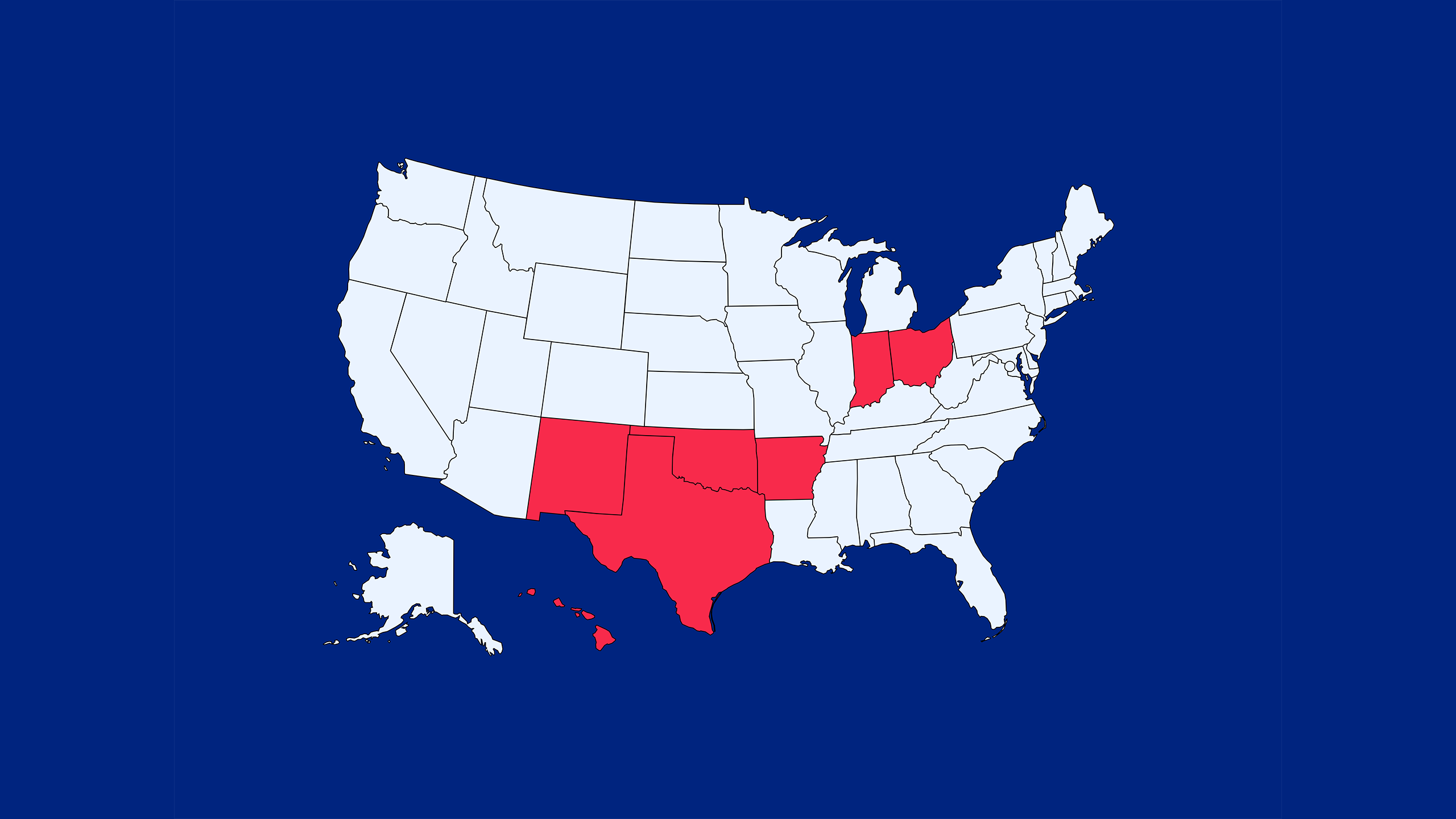
2025 Outbreaks and/or Confirmed Cases in the U.S.
January and February 2025: Texas and New Mexico
The first measles outbreak of this year began in January 2025 in Gaines County, Texas.
March 2025: New Mexico, Texas and Oklahoma
The first death from measles was reported in Lubbock, Texas, in February 2025 — the first in the U.S. since 2015.
April 2025: Arkansas, Hawaii, Indiana, Texas, New Mexico, Ohio and Oklahoma
By April 2025, measles had been reported in seven U.S. states, with cases inching closer to 1,000.
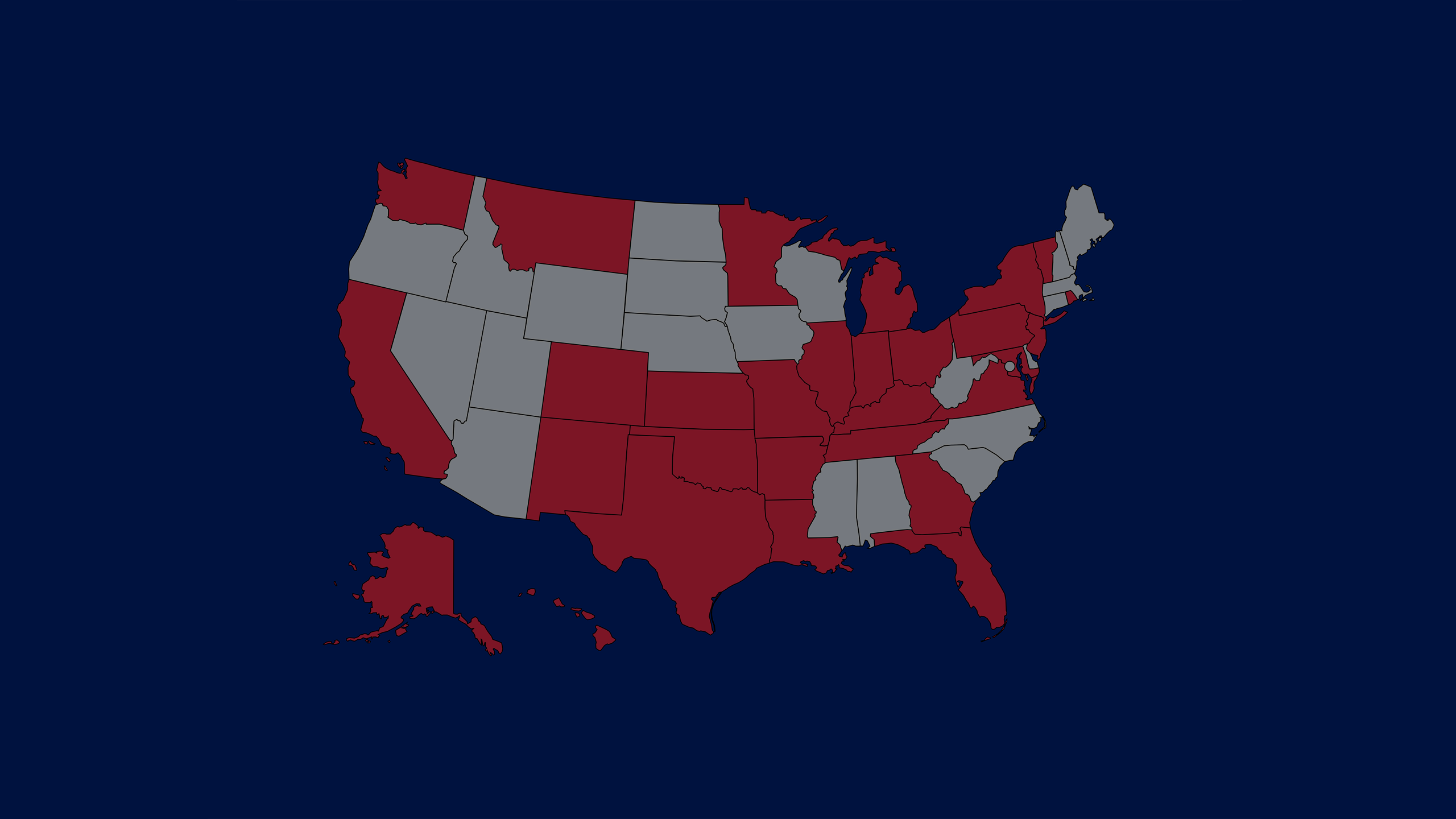
As of April 30, 2025, 30 states have reported measles cases
96% of the total cases reported have been in unvaccinated people.
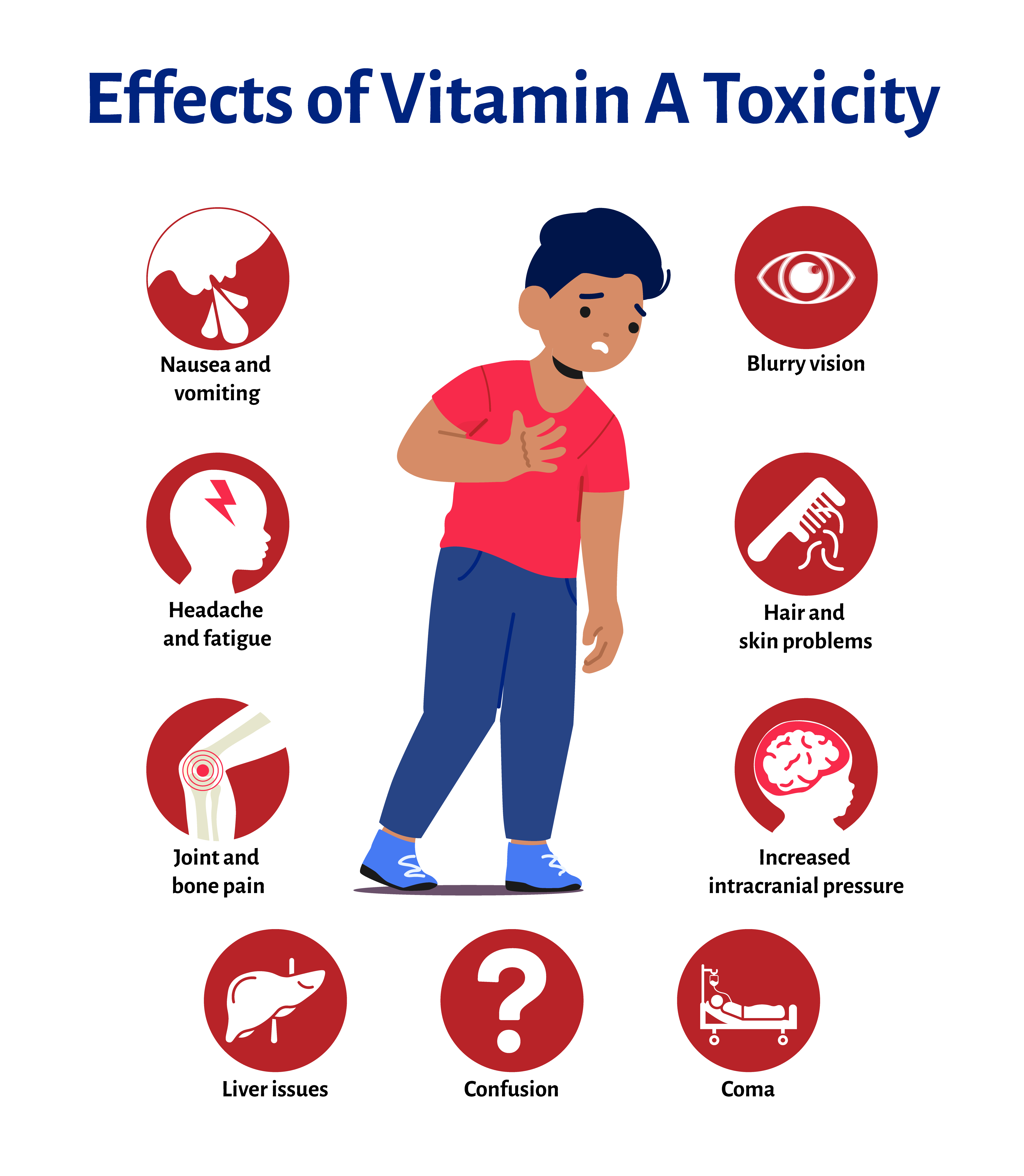
In addition to working to vaccinate and treat children, pediatricians also are debunking claims that certain treatments, including vitamin A, can prevent measles.
During a measles infection, the virus depletes vitamin A in the body. Vitamin A deficiency can cause eye damage and blindness. When the body doesn't have enough vitamin A, it may also increase the risk of serious illness and death from measles.
“Vitamin A is recommended for children diagnosed with measles to help prevent complications, particularly in children who are hospitalized,” said Sean T. O’Leary, M.D., M.P.H., FAAP, chair of the AAP Committee on Infectious Diseases.
“Vitamin A should not be used to try to prevent measles, and high doses of vitamin A are potentially very harmful. The only effective way to prevent measles is the MMR vaccine.”
Many U.S. experts concur with administering vitamin A to all children in the United States with measles, regardless of hospitalization status, according to the AAP Red Book. While there is no specific antiviral treatment for measles, the World Health Organization recommends two doses of vitamin A be administered by a health care professional 24 hours apart for children and adults with measles.
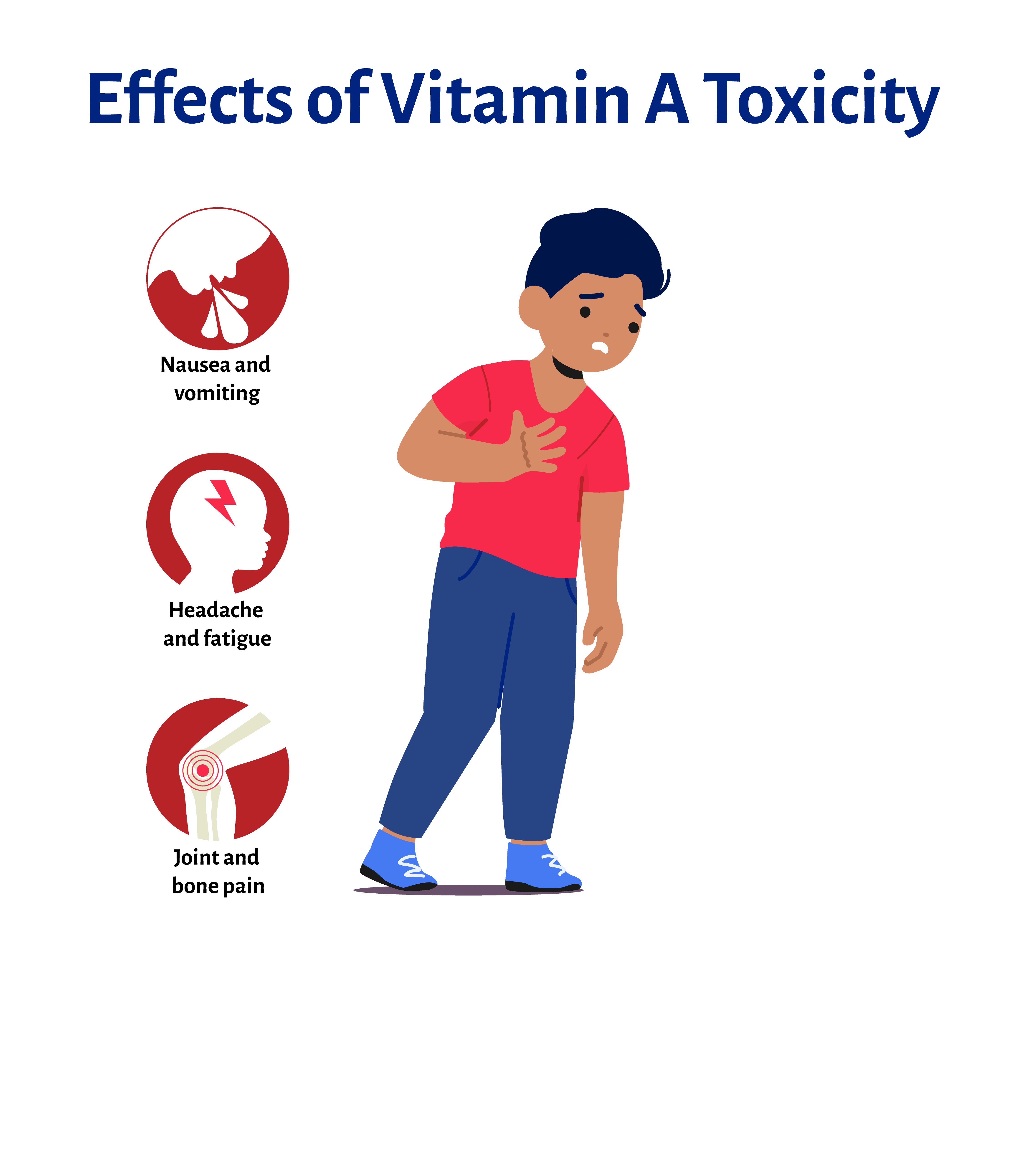
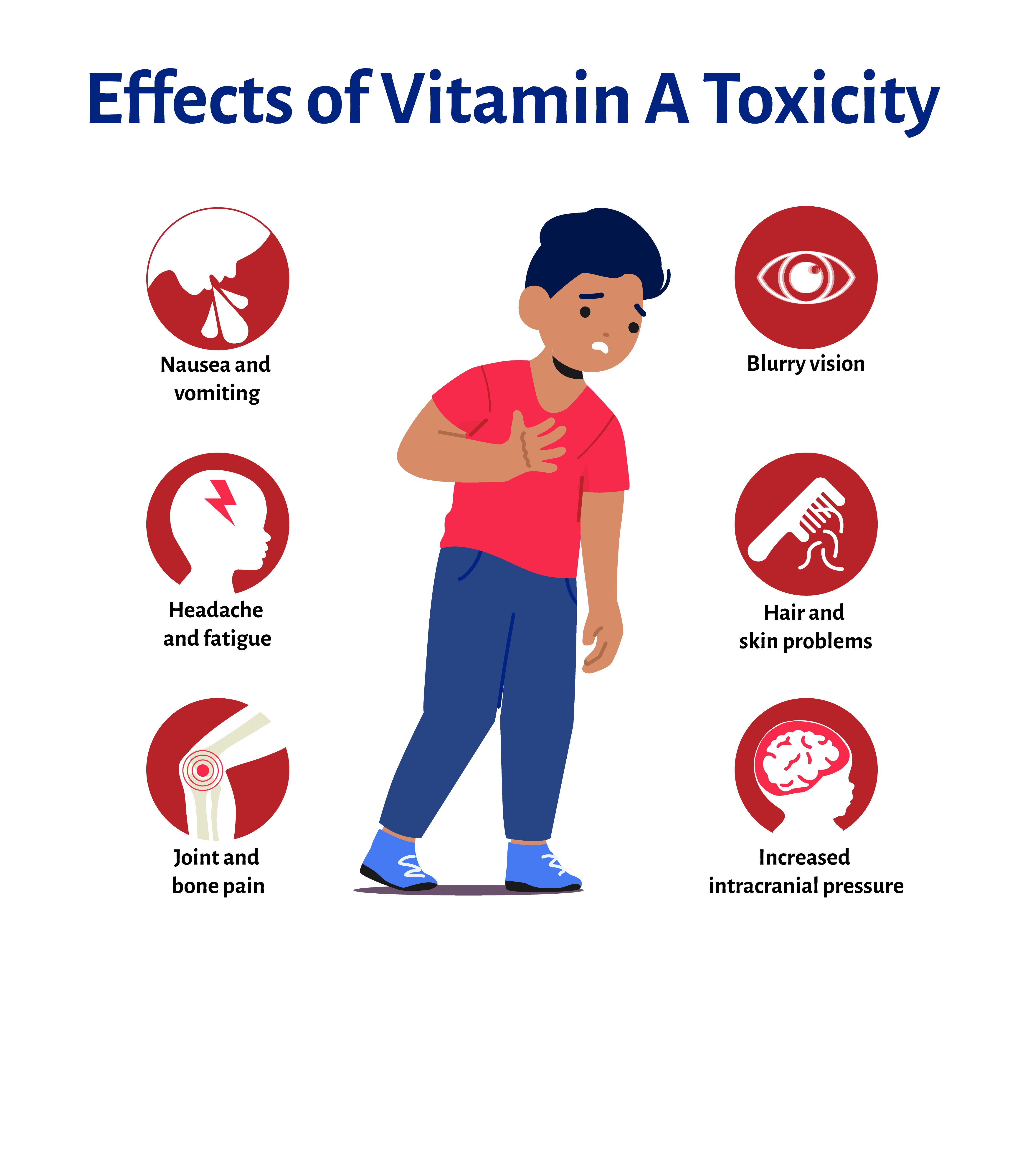
This information may have led some to believe vitamin A can prevent measles. Larger, prolonged doses of vitamin A can cause nausea and vomiting, headache and fatigue, joint and bone pain, blurry vision and skin and hair problems. This also can lead to dangerously high pressures inside the skull that push on the brain, liver damage, confusion, coma and other problems.
When to Vaccinate
The AAP and the Centers for Disease Control and Prevention (CDC) recommend children receive the MMR vaccine at age 12–15 months and again at 4–6 years. Two doses are 97% effective against measles.
Pediatricians should follow state and local guidance on early administration of MMR vaccine doses.
12–15 months of age
Infants 12 through 15 months receive the first dose of measles, mumps, rubella (MMR) vaccine.
4–6 years of age
A second dose of MMR is given at 4 to 6 years of age. For additional MMR guidance, refer to the measles chapter in the Red Book.
Teenagers and adults
Teenagers and adults with no evidence of immunity should receive one dose of MMR vaccine immediately and follow with a second dose at least 28 days later.
Post-exposure vaccination
MMR can be used as preventive care if administered ≤ 72 hours after measles exposure in individuals 6 months of age and older who do not have evidence of measles immunity.
Dr. Cvijanovich recalls treating a teenager in the early 2000s who became infected with measles as an infant after being exposed to an unvaccinated child. The patient later developed long-term effects of the initial measles infection.
“I happened to be there the night he was admitted to get a spinal tap to see if he indeed had the measles virus in his spinal fluid,” Dr. Cvijanovich said. “And I was there the night about a year-and-a-half later when he died of aspiration pneumonia, and he was at that point neurologically devastated. It was horrible watching this perfectly delightful 13-year-old slowly, slowly die. The choices another child’s parents made took away this child from their family.”
Dr. Cvijanovich shares the story with her families to promote vaccination. While many are moved by her experiences, some still refuse immunizations. Still, she encourages her peers to use any and all opportunities with families to discuss vaccination to protect the larger community.
Listen to Dr. Cvijanovich share this story.
"One death from a preventable disease is one too many."
Visit the original article on AAP News by Steve Schering, staff writer:
Measles outbreak provides opportunities to discuss vaccination with families
More resources
Measles Toolkit, American Academy of Pediatrics
Use the tools and resources in this toolkit to help promote timely measles vaccination and combating misinformation.
Measles Cases and Outbreaks, Centers for Disease Control and Prevention
This page shows a regularly updated count of measles cases and outbreaks in the United States as well as answers to frequently asked questions from the CDC.
Recommendations for Vaccinations, American Academy of Pediatrics
This page contains more information on the AAP's recommendations on measles vaccination, updated treatment policies, and resources for families.